Early diagnosis begins with a medical history and involves using neuroimaging, standardized neurological, and standardized motor assessments that indicate congruent abnormal findings indicative of cerebral palsy. Clinicians should understand the importance of prompt referral to diagnostic-specific early intervention to optimize infant motor and cognitive plasticity, prevent secondary complications, and enhance caregiver well-being.
The National Institute of Neurological Disorders (NINDS) and the National Institute of Child Health and Human Development (NICHD) are hosting a national cerebral palsy research workshop that will help develop the next US strategic plan for cerebral palsy research, to be held virtually on August 17 and 18.
CPF Executive Director Rachel Byrne and Chris Modlesky, PhD discuss exercise, fitness, research, research funding and his current research.

CPF Executive Director Rachel Byrne and Jocelyn Cohen, Vice President of Communications and Engagement at Cerebral Palsy Alliance Research Foundation discuss collaboration in research.

Students with disabilities often need extra support throughout the day to access their environment, the academic materials, and learn alongside their peers. A Personal Care Attendant in the school setting is often utilized to support the students needs.

Children and teens with cerebral palsy and other disabilities may need the assistance of an individual who has a background in healthcare and the skills to provide the services essential to quality care.

Personal Care Attendants for adults with cerebral palsy and other disabilities provide a variety of essential functions that ensure safety, health, wellbeing and overall impact quality of life.

An employment agreement spells out the rules, rights and responsibilities for both the Personal Care Attendant (the employee) and the individual with cerebral palsy or family who is hiring the Personal Care Attendant.

Author David Stoner provides insight into his experience with Personal Care Attendants through the years as his needs and his family's needs have changed.

On this episode, I have the honor of talking with Wendy Pierce, MD, a pediatric physiatrist at Colorado Children's Hospital about physiatry, also known as Physical Medicine and Rehabilitation. This fantastic field of medicine can be helpful for individuals with cerebral palsy across with lifespan, but it has a confusing name and sometimes a confusing job description. So we set out to help listeners better understand what a physiatrist does.
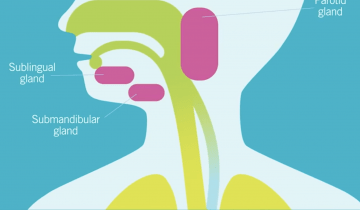
Drooling is an important problem for many individuals with CP and there are a number of interventions available to treat symptoms. If an individual with CP or their caregiver have concerns about drooling it is important to discuss with a health care provider. Care pathways such as the AACPDM pathway can be a starting point for shared decision making. In all cases, working together as a team is important in choosing the best alternative. Children and adults with CP may have trouble with drooling, or saliva management. In the medical world, drooling is referred to as sialorrhea. Saliva plays an important role in eating but also can interfere with airway clearance and breathing, as well as social participation. When drooling has this kind of impact it becomes important to consider intervention.

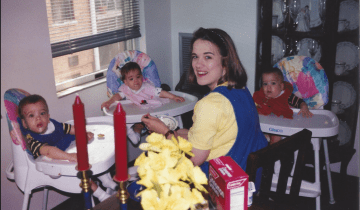
My boys were exactly the same amazing, lovable, adorable, brilliant little boys after the diagnosis, that they had been before it. The exact same.
Many children with cerebral palsy (CP) have difficulty controlling saliva. Drooling varies in severity and can be distressing for the children, families and caregivers. Chronic drooling is referred to as Sialorrhea and occurs as a result of limitations in a person’s ability to control and swallow oral secretions.
Our “Let’s Talk CP” podcast series kicks off with a great conversation about what questions to ask your child’s clinician when your child has cerebral palsy. How should you prepare for a medical appointment? What questions should you ask? Should you get a second opinion? Join Cerebral Palsy Foundation host, Cynthia Frisina as she shares candid talk, lessons learned and great advice with fellow moms, Wendy Sullivan and Jennifer Lyman. This episode is made possible with the support of Ipsen Biopharmaceuticals.

The typical cognitive assessments that are used for children require them to be able to use their hands to point to pictures or hold puzzle pieces.

There is insufficient research on adults living with cerebral palsy, (as referenced in my previous blog post on cerebral palsy and adulthood). Although there is a paucity of studies examining mental health in this population, medical researchers have speculated that the rate of depression is three to four times higher in people with disabilities such as CP than it is in the general population.

"Cerebral palsy is primarily a motor impairment so it's really important to look at what the child’s motor function is. Are they developing on the trajectory of a child who has cerebral palsy or are they developing as we would expect a baby to develop? "

When first meeting a parent who's had a child newly diagnosed with cerebral palsy, I really want to try and help them understand their baby. It can be difficult for parents to take it in all at once and many leave that first interview quite overwhelmed, but you're going to meet some really important and helpful people.
Sleep is important to all of us, but it's especially important for infants. When infants go to sleep, they start to create neural networks about what they've been learning during the day. It's estimated that as many as one in five children with disabilities have a sleep disorder, and that's higher than the rate of typically-developing children. Finding sleep interventions for these children is incredibly important so they can lay down their brain networks and continue to learn during their early childhood years.

Receiving early diagnoses or high‐risk for CP classification is a parent priority. Alignment between parents and providers exists for International Classification of Function domains of body functions/structures and activity, but less for those of environment, personal, and participation.
My name is Nathalie Maitre, I work at Nationwide Children's Hospital. I'm a physician and a researcher

Owen is our third baby and after a healthy pregnancy and making it to 38 weeks, I thought we would coast into life with three kids and adapt to the beautiful chaos that is life outnumbered by little ones. Somewhere in between, I ended up watching as my newborn baby was packed up into a life-flight helicopter and whisked away before I even got a chance to hold him. I would do whatever it took to get to Owen at Nationwide Children’s Hospital, I would will him from hundreds of miles away to hang on, to fight long enough for me to get there – and then we could do “whatever it took” together.

Children with cerebral palsy experience brain damage around birth or before birth. So the language of the brain in other words, the way they will move, will be different from typical movements. So by looking at their movements, we will understand that there is something that is wrong in the brain.