This recent study found that over half of children and young people with Cerebral Palsy have more than one movement disorder, which is more common than previously thought.
Dr. Heather Riordan explains how different motor types can occur at the same time in some people and how to decide what to treat first.

Neurologist and movement disorder specialist, Heather Riordan, MD, describes the Chorea in Cerebral Palsy and what to do if it is impacting your function.
Do you or your child have movements that are difficult to control? Is your mobility and function impacted by abnormal movements or do these movements cause pain? If so, you or your child may have Dyskinesia. If you want to learn more, including how it is treated, don't miss this educational Town Hall with experts Dr. Heather Riordan, from Kennedy Krieger Institute, and Dr. Michael Kruer, from Phoenix Children's.

CPF Executive Director Rachel Byrne and Dr. Heather Riordan, Director of the Phelps Center for Cerebral Palsy at the Kennedy Krieger Institute discuss dyskinesia.

The Dyskinetic Cerebral Palsy Functional Impact Scale is a new tool useful measuring the functional impact of dyskinesia on children's movements and postures and the perceived impact of dyskinesia on daily activities. It can can help identify priorities for intervention.
This systematic review looks at all available evidence for pharmacological/neurosurgical interventions for managing dystonia in individuals with cerebral palsy to inform the AACPDM care pathway.
Hypotonic CP, also known as hypotonia, is a form of cerebral palsy that causes low muscle tone. In other words, the muscles are overly relaxed and your child may feel floppy.
Mixed types of CP refer to symptoms that don’t correspond to any single type of CP but are a mix of types. For example, a child with mixed CP may have some muscles that are too tight and others that are too relaxed.

Ataxia affects balance and depth perception. Children with ataxia will often have poor coordination and walk unsteadily with a wide-based gait.
Dyskinesia is an umbrella term encompassing a range of different movements. These are all movements that can be out of your control. Dyskinesia is very common in cerebral palsy.

Dr. Bhooma Aravamuthan presents Understanding Dystonia: Diagnosis and Treatment at the 2020 AACPDM Community Forum. Moderated by Council Chair, Jen Lyman.
The Dystonia Care Pathway was updated in 2024 based on best available evidence. The goal of the these Care Pathways is to help Health Care Professionals understand the research evidence on the topic so that they can make clinical decisions for the care of the individual.
Spastic cerebral palsy is the most common type of CP. People will experience increased muscle tone and their movements may appear stiff or awkward.
People who have dyskinetic cerebral palsy experience involuntary movements that are difficult to control. These movements can be slow, twisting and writhing, or rapid and jerky, and can impact movement in the hands, arms, feet, legs and even the face or tongue.
Do you or your child have movements that are difficult to control? Is your mobility and function impacted by abnormal movements and cause pain? If so, you or your child may have Dyskinesia. If you want to learn more, including how it is treated, please join us on for a new educational Town Hall with experts Dr. Susan Biffl, from Rady Children's Hospital, and Dr. Mark Gormley, from Gillette Children's.
Students with disabilities often need extra support throughout the day to access their environment, the academic materials, and learn alongside their peers. A Personal Care Attendant in the school setting is often utilized to support the students needs.

Children and teens with cerebral palsy and other disabilities may need the assistance of an individual who has a background in healthcare and the skills to provide the services essential to quality care.

Personal Care Attendants for adults with cerebral palsy and other disabilities provide a variety of essential functions that ensure safety, health, wellbeing and overall impact quality of life.

An employment agreement spells out the rules, rights and responsibilities for both the Personal Care Attendant (the employee) and the individual with cerebral palsy or family who is hiring the Personal Care Attendant.

Author David Stoner provides insight into his experience with Personal Care Attendants through the years as his needs and his family's needs have changed.

On this episode, I have the honor of talking with Wendy Pierce, MD, a pediatric physiatrist at Colorado Children's Hospital about physiatry, also known as Physical Medicine and Rehabilitation. This fantastic field of medicine can be helpful for individuals with cerebral palsy across with lifespan, but it has a confusing name and sometimes a confusing job description. So we set out to help listeners better understand what a physiatrist does.
My boys were exactly the same amazing, lovable, adorable, brilliant little boys after the diagnosis, that they had been before it. The exact same.
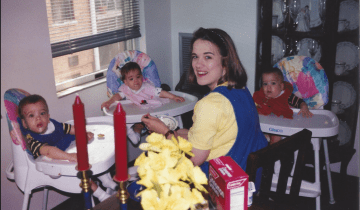
Our “Let’s Talk CP” podcast series kicks off with a great conversation about what questions to ask your child’s clinician when your child has cerebral palsy. How should you prepare for a medical appointment? What questions should you ask? Should you get a second opinion? Join Cerebral Palsy Foundation host, Cynthia Frisina as she shares candid talk, lessons learned and great advice with fellow moms, Wendy Sullivan and Jennifer Lyman. This episode is made possible with the support of Ipsen Biopharmaceuticals.


