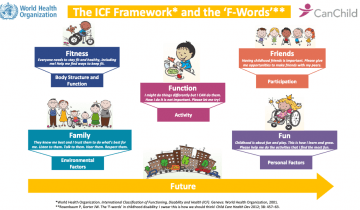
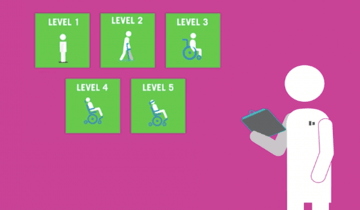
CP describes a spectrum of conditions that affects individuals in many different ways. Your care team may use the term GMFCS which stands for Gross Motor Function Classification Scale and is used to describe what mobility aids your child may need to complete certain tasks.