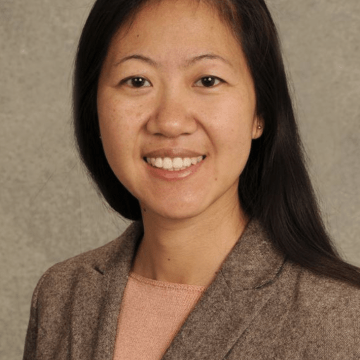
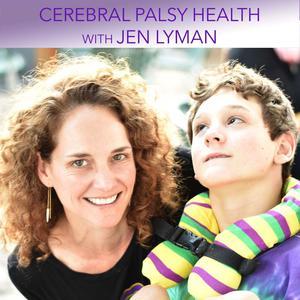
Cerebral Palsy Health with Jen Lyman
Cerebral Palsy is a complex health condition that impacts each individual differently. As a result, finding information about what might help improve function, increase participation, and achieve health and lifestyle goals can be difficult. This podcast is a place for conversations with experts about issues related to cerebral palsy that affect health, fitness, function and participation. We will cover a range of topics including: treatments and therapies, nutrition, neuroplasticity, genetics, exercise and fitness, adaptive sports, accessibility, and new trends.
-

Episode 15: Understanding Vision with Belinda Deramore Denver, PhD, OT -

Episode 14: Cerebral Palsy Research Advocacy with Cynthia Frisina -

Episode 13: Oral Health and Dentistry with Drs. Erica Caffrey and Sydnee Chavis -

Episode 12: Sleep Issues and Solutions for CP with Dr. Golda Milo-Manson -

Episode 11: Participation with Nathan Rosenberg, MD -

Episode 10: Early Detection and Intervention with Dr. Nathalie Maitre -

Episode 9: The Ins and Outs of Powered Mobility with Dr. Lisa Kenyon -

Episode 8: Cerebral Palsy Health. Disability and Employment with Sarah Storck and David Stoner -

Episode 7: Cerebral Palsy Health. Noam Platt - Makers Making Change -

Episode 6: Cerebral Palsy Health. Theresa Sukal Moulton, PT, DPT, PhD and David Black: Frame Running an Adaptive Recreational Sport for Individuals with Cerebral Palsy -

Episode 5: Cerebral Palsy Health. Wendy Pierce, MD: What Does a Physiatrist Do Anyway? -

Episode 4: Cerebral Palsy Health. Iona Novak, PhD and Madison Paton, PhD: What's the Deal with Stem Cells Anyway? -

Episode 3: Cerebral Palsy Health. Amy Bailes, PhD, PT, PCS: ABC's of CP -

Episode 2: Cerebral Palsy Health. Mary Gannotti, PhD, PT: Fitness, Health and Function Across the Lifespan for Individuals with Cerebral Palsy -

Episode 1: Cerebral Palsy Health. Meet Your Host - Jen Lyman
-

CPH - Coffee Talk Episode 5 with Dr. Nathalie Maitre: Preventive Care and Vaccines In Episode 5 of Coffee Talk, Nathalie and Jen discuss preventive care and vaccines. -

CPH - Coffee Talk Episode 4 with Dr. Nathalie Maitre: Research In Episode 4 of Coffee Talk, Nathalie and Jen discuss research and clinical trials. -

CPH - Coffee Talk: Episode 3 with Dr. Nathalie Maitre: Fitness In Episode 3 of Coffee Talk, Nathalie and Jen discuss their experiences with fitness for their sons with CP. -

CPH - Coffee Talk: Episode 2 with Dr. Nathalie Maitre: Sleep In Episode 2 of Coffee Talk, Nathalie and Jen discuss their experiences with sleep as it has impacted their sons and their lives. -

CPH - Coffee Talk Episode 1 with Dr. Nathalie Maitre: CP Parenting and Mental Health In this new series within Cerebral Palsy Health, Jen sits down with Nathalie Maitre, MD, PhD to talk about parenting, our shared experiences raising sons with CP and more!