Making informed decisions about care and treatment for cerebral palsy (CP) can be overwhelming, especially with the vast amount of medical research available. Through this guide, we aim to help you better understand the types of research you may encounter and provides practical tips for evaluating studies relevant to CP.
Dental Professors, Dr. Erica Caffrey, DDS and Dr. Sydnee Chavis, DMD, MS discuss oral health and dentistry across the lifespan.

In Episode 4 of Coffee Talk, Nathalie and Jen discuss research and clinical trials.

Our research shows that higher Bone Mineral Density (BMD) was associated with a greater risk of fracture, which is opposite of what we would expect. When we picked apart the BMD ratio we found that bone size had the strongest association with fracture risk, such that smaller bones had a greater risk.
CPF Executive Director Rachel Byrne and Chris Modlesky, PhD discuss exercise, fitness, research, research funding and his current research.

Good nutrition is critical for your child's healthy brain development. It's not uncommon for families to struggle getting enough food to eat. If you feel like you haven't had enough food to feed your whole family in the last month, please talk to someone. This is a common problem.

CPF Executive Director Rachel Byrne and Jocelyn Cohen, Vice President of Communications and Engagement at Cerebral Palsy Alliance Research Foundation discuss collaboration in research.

Drooling is an important problem for many individuals with CP and there are a number of interventions available to treat symptoms. If an individual with CP or their caregiver have concerns about drooling it is important to discuss with a health care provider. Care pathways such as the AACPDM pathway can be a starting point for shared decision making. In all cases, working together as a team is important in choosing the best alternative. Children and adults with CP may have trouble with drooling, or saliva management. In the medical world, drooling is referred to as sialorrhea. Saliva plays an important role in eating but also can interfere with airway clearance and breathing, as well as social participation. When drooling has this kind of impact it becomes important to consider intervention.

Many children with cerebral palsy (CP) have difficulty controlling saliva. Drooling varies in severity and can be distressing for the children, families and caregivers. Chronic drooling is referred to as Sialorrhea and occurs as a result of limitations in a person’s ability to control and swallow oral secretions.
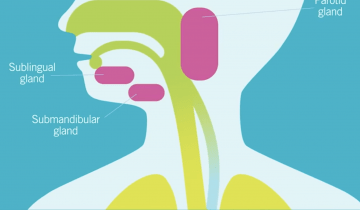
Oropharyngeal dysphagia, or OPD, is an impairment of the oral or pharyngeal phases of the swallow. This can impair muscle movements and coordination of the mouth, such as the lips, tongue, jaw, cheeks, palate, and also muscles of the pharynx and the entry to the airway.

Weight, height and body composition are important indicators for development. The tools used to measure these can be different for children with cerebral palsy.

Children with cerebral palsy (CP) often grow poorly and assessment of growth in this population is further complicated by two main difficulties. Firstly, children may have joint contractures, muscular weakness, scoliosis, and/or involuntary movements that make standing or lying straight difficult, if not impossible.
When we have a physical disability, our bones can get a bit weak or osteoporotic. Something that can be improved is promoting bone health for people with cerebral palsy.