Considering the Alternatives: A Guide to Choosing Treatments and Therapies
Cerebral palsy (CP) affects movement, muscle tone, coordination and more. Importantly, CP is unique to each individual and may look and feel differently across the lifespan. Along the way, families and individuals with CP often explore a variety of treatment options and therapies to improve function, decrease the impact of disability, or increase participation and improve quality of life. Navigating treatments and therapies, including traditional, complementary and /or alternative, requires careful consideration to ensure safety, efficacy, and alignment with individual needs, including your time. Our aim is to provide a framework for evaluating these therapies, emphasizing critical thinking and informed decision-making. We encourage you to be curious, know your goals and keep in mind that research evidence is evolving.
Overview of Conventional Medicine and Therapies for Cerebral Palsy
Conventional medicine for cerebral palsy refers to treatments that are widely accepted and practiced by medical professionals, including physicians, therapists, and allied health providers. This includes medications, various forms of therapy (physical, occupational, speech), surgery, and assistive devices, all delivered by a coordinated team of healthcare professionals. Many of these treatments are supported by scientific evidence and may have clinical guidelines which have clear indications for whom they may serve to benefit. It is important to note that this is not always the case and you should carefully assess whether a treatment or modality offered by a conventional provider has the evidence to support your needs or goals.
Main Categories of Conventional Treatments and Therapies
- Medications - Muscle relaxants; Botulinum toxin injections; Anticonvulsants are used for co-occurring epilepsy or seizures or other medications may address associated symptoms like drooling or pain.
- Physical Therapy - Focuses on exercises and activities to improve function, muscle strength, balance, coordination, and mobility.
- Occupational Therapy - Helps to develop skills for daily living, such as dressing, eating, and participating in school activities.
- Speech and Language Therapy - Assists with speech clarity, communication, and swallowing difficulties and AAC devices.
- Recreational Therapy – Recreation, Adaptive Sports and Leisure skills development, such as arts, games, sports, fitness and cultural activities aim to enhance physical, social and intellectual abilities.
- Surgical Interventions – Orthopedic and Neurosurgeries for spasticity, contractures, or orthopedic deformities.
- Assistive Devices - Orthotics, braces, walkers, wheelchairs, communication aids, and other adaptive equipment.
Alternative AND Complementary Treatments and Therapies (CAMS)
Many people use health care methods outside of conventional Western medicine. The terms "alternative" and "complementary" are often used interchangeably and together they are called CAMs, but they have different meanings - Complementary Therapies are non-mainstream approaches used alongside conventional medical treatments. They can enhance traditional therapies without replacing them. Alternative Therapies are non-mainstream approaches used instead of or to replace conventional treatments. They often lack scientific evidence and some may require or suggest abandoning established therapies.
Main Categories of Complementary and Alternative Treatments and Therapies:
- Nutritional: Special diets, supplements, probiotics or herbs
- Psychological: Meditation, relaxation, mindfulness
- Physical: Swimming, Pilates, massage
- Mind-Body: Yoga, Tai-chi, acupuncture, biofeedback, Feldencrais Method
- Energy Healing: Reiki, Qigong
- Sensory: Art, Dance, or Music therapies, or sound baths and aromatherapies
HOW TO EVALUATE THERAPIES
When considering a therapy, begin by asking yourself these important questions:
1. Source and Claims:
- Who is promoting the therapy? Is it a reputable source (like your doctor or therapist) or a personal anecdote? If it is a personal anecdote, does this person have similar symptoms or goals that you are trying to achieve?
- Are the claims too good to be true? Do they promise to cure or improve multiple (unrelated) symptoms?
- Consider the source (where did you learn about the treatment or therapy): social media, friend, therapist, or peer-reviewed research article such as a Systematic Review or Meta Analysis.
2. Goals and Measurement:
- Is the therapy goal-oriented, and does it involve self-initiated movements or is it passive?
- What are the specific goals of the therapy or treatment?
- Are the goals aligned with your goals for your child or yourself? Specifically and realistically - are these goals designed to meet the needs based on type of CP and/or limbs impacted (or other specific need)?
- How will progress be measured? Are there clear, achievable milestones?
3. Safety and Efficacy:
- Is the treatment or therapy safe? Are there any potential risks or side effects? How do you know?
- What evidence supports its effectiveness? Is it based on peer-reviewed research or anecdotal evidence?
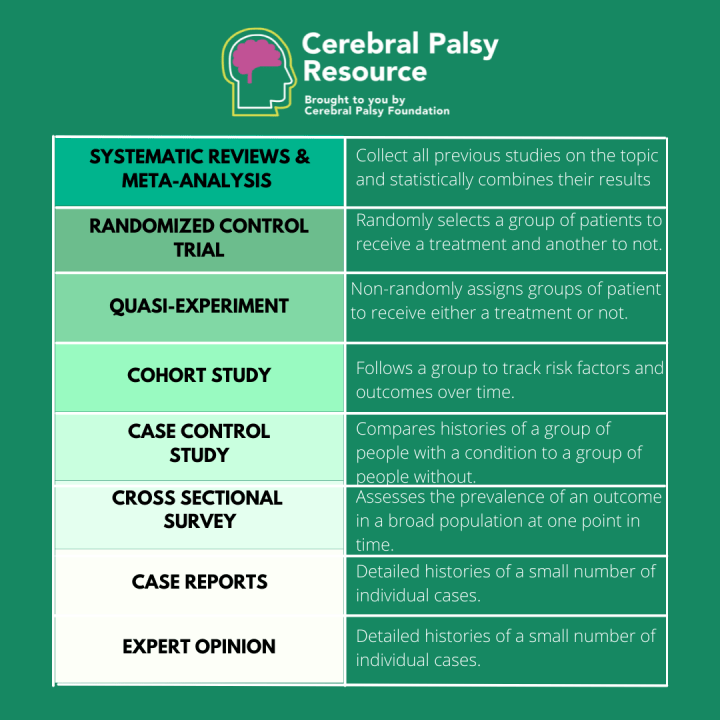
- Evaluate the strength of evidence using the evidence pyramid: systematic reviews and meta-analyses are at the top (preferred), followed by randomized controlled trials (RCTs), then observational studies.
4. Cost and Commitment:
- What are the financial costs? Will you have to fund raise, take out a loan or borrow to afford this?
- Is it covered by insurance? Will you have to submit for insurance reimbursement or does the provider do this?
- Are there financial assistance options?
- Are there any hidden costs, such as travel or equipment expenses?
- What is the time commitment? Does it require frequent travel, long distances, or outside the country?
5. Practicality and Fun:
- Is the therapy enjoyable? Does it promote engagement and motivation?
- Is it functional and does it involve self initiated movements?
- Can skills learned in therapy be practiced at home, or does it rely on specialized equipment or expertise?
RED FLAGS
Is the treatment science or snake oil? When evaluating treatments and therapies, there are a few red flags that you should pay close attention to before you buy in:
- Proprietary Therapies: Be cautious of therapies named after their creators, requiring exclusive use, signing non disclosure agreements or liability waivers.
- Lack of Peer-Reviewed Research: Ensure that any claims are backed by studies published in reputable journals.
- Pressure to Abandon Other Therapies: Be wary if you're advised to stop conventional treatments without a valid reasons.
- Unrealistic Promises: Therapies claiming to cure or vastly improve multiple symptoms may be overly optimistic.
- Your Gut Instinct: Does this feel right to you? Do you feel comfortable discussing with your doctor or with trusted loved ones? Can you describe what is happening in the therapy?
CRITICAL THINKING AND DECISION-MAKING
- Consult with Healthcare Providers: Discuss potential therapies with your child's healthcare team to ensure they align with existing treatments.
- Know your Goals: It is important to know what exactly you aim to achieve by embarking on this treatment or therapy to ensure the goals align.
- Evaluate Research: Look for systematic reviews and meta-analyses, which provide the highest level of evidence. Randomized Controlled Trials (RCTs) are also highly valued for assessing efficacy.
- Consider Personal Stories with Caution: While personal experiences can be inspiring, they may not apply to your child's unique situation.
- Stay Informed: Continuously update your knowledge on the latest research and therapies to make informed decisions.
You Decide to Go For it...What next?
You (and hopefully your provider) decide a supplement, new medication, therapy or treatment intervention is not going to hurt, but how can you tell it is helping?
- Look for clinical trials looking at this treatment or therapy (visit clinicaltrials.gov)
- Keep Key People Blind to the intervention (don't tell close friends or relatives, teachers or therapists about it and see if they notice any differences or changes)
- Be sure to know the desired effect or goal
- Decide on a time frame – 3 months? 6 months?
- Don’t change any other factors
QUESTIONS TO ASK YOUR PRIMARY HEALTHCARE PROVIDER or Provider who manages your Cerebral Palsy
Consulting with your healthcare provider can be very helpful in sorting through safety and efficacy, they also may have other patients and families who have had also tried the same treatment or therapy who are willing to share their experiences.
Be sure to review with your provider these key questions:
- Is this therapy safe?
- What evidence supports its safety and effectiveness for cerebral palsy?
- Are there any potential interactions with current medications or therapies?
- Have there been any clinical trials or research studies?
- Are there any clinical trials or ongoing research that we can participate in?
- How does this therapy align with our current treatment plan?
- Can it be used alongside current therapies, or should we stop other treatments?
- Are there any risks associated with discontinuing current therapies?
- Is this treatment/ therapy accessible in our area, or will we need to travel?
- How often will sessions be needed, and what is the expected duration of treatment?
- Can skills learned in therapy be practiced at home, and/or does it require specialized equipment?
- How will we measure the effectiveness of this therapy?
- What are the expected outcomes, and how will we assess them?
Questions to ask the Therapist or Treatment Provider
Whether you are interviewing a surgeon, a physical therapist or an alternative provider such as an acupuncturist or yoga therapist, these questions can help you determine if their experience and the treatment matches your needs:
- Qualifications and Experience:
- Treatment or Therapy Details
- Safety and Risks
- Evidence and Research
- Costs and Logistics
- Communication with Healthcare Providers
- Goals and Progress Monitoring
- Home Practice and Carry Over
- What qualifications do you have to provide this therapy?
- How long have you been practicing this therapy, and what experience do you have with individuals with cerebral palsy?
- What exactly happens during a therapy or treatment session?
- How does this address my child's specific needs and goals?
- Are there any specific techniques or methods used, and how do they work?
- Are there any potential risks or side effects associated with this therapy or treatment?
- How do you ensure safety during treatment sessions, especially if there are other health conditions?
- What evidence supports the SAFETY and EFFECTIVENESS of this therapy for cerebral palsy?
- Are there any published, peer reviewed studies or research papers that you can share?
- What are the costs of this therapy, and are there any discounts or packages available?
- How often will sessions be needed, and how long will each session last?
- Are there any additional costs for equipment or travel?
- Are you willing to communicate with my child's healthcare providers to ensure coordination of care?
- How will you keep them informed about progress or any changes?
- What are the specific goals of this therapy for my child?
- How will progress be measured, and what milestones should we expect?
- Can skills learned in therapy be practiced at home, and if so, how?
- Are there any resources or support for continuing therapy at home?
Examples of CAMs offered for Cerebral Palsy
Below are some of the more common Complementary and Alternative treatments and therapies that families inquire about and seek out:
- Anat Baniel Method
- Cannabidiol (CBD)
- Conductive Education
- Craniosacral Therapy
- Dynamic Movement Intervention
What is the intervention?
Created by Anat Baniel, a protégé of Moche Feldencrais, developed her neuromovement technique, a series of movement exercises, that claims to incorporate the "Nine Essentials" or learning principles of neuroplasticity.
How does it work?
- Series of movement exercises to promote neuroplasticity during which a practitioner physically guides the child/individual through movements, the idea is for them to experience the feeling of subtle differences the brain requires to form new connections and create new movement patterns. .
- Groups of 5-10 ”lessons” are delivered in a 2 week intensive period. Sometimes with 2 ”lessons” per day with breaks in between and breaks in between "intensives".
Who is it for?
Children and adults with neurological differences.
Is it safe?
This is a primarily passive and gentle movement experience which appears to be safe, however there is no research to demonstrate safety.What is the data?
- NO DATA, NO PUBLISHED RESEARCH
- Uses information about the principles of neuroplasticity to make claims about the intervention's effectiveness, to be clear, this is not research on her intervention.
This absence of evidence means there is no way to evaluate the safety, effectiveness, or credibility of the treatment. Without publicly available results or peer-reviewed publications, the scientific community has no means to validate the claims being made.
Considerations:
May involve considerable time, travel and cost commitment. Practitioners may recommend stopping other therapies.
- Depending on the experience of the practitioner, costs may range from $100 - $950 per lesson.
- Lessons last for approximately 30 minutes - 1 hour
- 1 - 2 times per day
- 2 Week Intensive Model
References:
There are no research studies on this intervention.
What is it?
A non-psychoactive cannabinoid found in the cannabis plant.
How does it work?
Interacts with cannabinoid receptors to modulate physiological functions.
Safety and Efficacy:
While it may reduce dystonia and spasticity, however studies are small and lack control groups.
What is the data?
One small study of 25 patients took CBD:THC 6:1 ratio or 20:1, they saw a reduction in dystonia and spasticity, however the study was not randomized, not blinded, there was no control group and a small study size.
Considerations: Consult with healthcare providers, consider legal implications, and monitor for side effects like sedation and liver toxicity.
References:
What is the intervention?
An Educational Model designed to teach movement and problem solving skills.
How does it work?
Utilizes specialized equipment, group dynamic, rhythmic intention, tasks, daily routines, and is typically led by a “Conductor” or teacher who has a 4 year certification from the Peto institute.
Who is it for?
Children and Adults with CP and other neurological disorders, like TBI or Stroke
Is it safe? Yes
What is the data?
- Prior to 2012, large state of evidence report of research comprising of studies from 1970’s- 2000 in general showed no difference in motor performance.
- Systematic review of early intervention showed no impact on motor performance.
- Current high quality RCT show no difference to conventional practice
- Newer studies looking at motor skills do have some promising results around motor learning.
Considerations: Families report a high level of satisfaction with Conductive Education camps and after school programs. Likely this is due to the intensity and community atmosphere and group dynamic of the classroom setting. The model utilizes specialized furniture and equipment that is expensive and may not transfer to a typical educational setting or home setting.
References:
Bourke-Taylor, H., O’shea, R., & Gaebler-Spira, D. (2007). Conductive Education: A Functional Skills Program for Children with Cerebral Palsy. Physical & Occupational Therapy In Pediatrics, 27(1), 45–62. https://doi.org/10.1080/J006v27n01_04
What is the intervention?
A type of osteopathic manipulative therapy, based on the controversial theory that the CNS (the brain and spinal cord) have subtle rhythmic pulsations that can be modified. Performed by osteopathic physician, some physical therapists and often chiropractors.
How does it work?
Stimulates healing using gentle hand pressure to manipulate the skeleton and connective tissues, especially the skull and sacrum (the large triangle at the base of the spine).
Who is it for?
Children and adults with a range of medical and disabling conditions such as migraines, asthma, TMJ. Some claim it is helpful for babies with birth trauma.
Is it safe?
- Potentially yes – Might be worth it for sleep, colic or constipation
- No – Adverse reactions reported for scoliosis and torticollis
What is the data?
A recent 2023 systematic review published in Chiropractic & Manual Therapies found no strong evidence that CST benefits children with cerebral palsy. The review looked at multiple randomized trials and concluded that most of the positive results came from poorly designed studies. When only high-quality evidence was considered, CST did not show any clear or consistent improvements in motor function. Researchers concluded that CST is not supported by reliable scientific data and should not be promoted as an effective treatment for cerebral palsy.
Sources:
What is the intervention?
Dynamic Movement Intervention (DMI) is a therapeutic technique used in physical and occupational therapy to treat children with motor delay by improving automatic postural responses and promoting progress towards developmental milestones (source – DMI website)
Who is it for?
Babies and children with neurodevelopmental disabilities such as CP or other disabilities
How does it work?
Therapist moves the child’s body through a series of chosen exercises or movements that will challenge the child’s neurological system against gravity
demonstrating safety and effectiveness of DMI for CP. Practitioners often make claims based on the “Principles of Neuroplasticity” or the ingredients that promote neuroplasticity, however the protocol has not been researched and evidence is anecdotal.
This absence of evidence means there is no way to evaluate the safety, effectiveness, or credibility of the treatment. Without publicly available results or peer-reviewed publications, the scientific community has no means to validate the claims being made.
- Often part of a 15 day "intensive treatment" sessions
- Costs vary from hourly (approximately $150 up) to daily rates that involve one or more therapies (approximately $500)
- Specialized equipment is needed
- Families often travel to locations where intensives are offered and stay locally during the treatment period (factor in hotel, AirB&B or other accommodations)
References:
There are no published research studies looking at the safety and effectiveness of DMI therapy
DMI Therapy (n.d.). DMITherapy.com. https://dmitherapy.com/
- Garment Suits/Adeli Suits
- Hyperbaric Oxygen Therapy
- Stem Cell Therapy
- Neurocytonics
- Neurodevelopmental Treatment (NDT)
What is the intervention?
The garment (clothing) that has elastic bands, ribbing or other structural or mechanical supports that is worn as an adjunct to therapy or intervention.
How does it work?
Depending on the type of suit, it might provide positioning support or alignment, proprioception or sensory feedback, or resistance
Who is it for?
Children with CP or other neurological deficits.
Is it safe?
Maybe - But children may experience overheating or some respiratory distress, so must be worn with supervision and removed immediately if any reactions occur.
What is the data?
- Systematic reviews have shown that garment therapy showed a nonsignificant effect on post-intervention function as measured by the Gross Motor Function Measure when compared to controls.
- Nonsignificant improvements in function were seen long-term.
- Garment therapy showed some improvement in postural stability
References
What is it?
Hyperbaric Oxygen Treatment (HBOT) involves breathing 100% oxygen through a mask while inside a sealed chamber that has been pressurized to greater than normal atmospheric pressure.
Who is it for?
Marketed towards individuals with CP, Traumatic Brain Injury, Stroke, Near Drowning
How does it work?
Elevates oxygen levels in the blood and brain. The mechanism involves elevating oxygen partial pressure in the arterial blood and improve oxygen tension in the hypoxic brain.
Is it Safe?
While safe for some conditions, its effectiveness for CP relies solely on case reports. Risks include ear problems in approximately 45% of participants, seizures and pulmonary complications.
What is the Data?
RCTs show no significant difference from pressurized room air.
2001 RCT published in the Lancet:
- 111 children with cerebral palsy aged 3–12 years were randomly assigned hyperbaric oxygen (n=57) or slightly pressurized room air (n=54).
- All children received 40 treatments over 2 months. Hyperbaric oxygen treatment was 1 h in 100% oxygen at 1·75 atmospheres absolute (ATA); children on slightly pressurised air received air at 1·3 ATA (the lowest pressure at which pressure can be felt, thereby ensuring the maintenance of masking).
- The main outcome measure was gross motor function. Secondary outcomes included performance in activities of daily living, attention, working memory, and speech.
- For all outcomes, both groups improved over the course of the study, but without any difference between the two treatments.
Considerations: Costs can be upward of $8000.00 for a series of treatments and not covered by insurance.
In addition, it is typically very time intensive, with each session lasting 60-80 minutes and sessions taking place 5 or 6 days of the week for a total of around 40 sessions.
Risks include ear problems and seizures. Ensure it aligns with your child's needs and consult with healthcare providers.
References:
McDonagh, M.S., Morgan, D., Carson, S. and Russman, B.S. (2007), Systematic review of hyperbaric oxygen therapy for cerebral palsy: the state of the evidence. Developmental Medicine & Child Neurology, 49: 942-947. https://doi.org/10.1111/j.1469-8749.2007.00942.x
What is it?
Cell replacement therapy utilizing stem-cells for the treatment of the insult or injury in the brain.
How does it work?
- Regenerative mechanisms – replacement or repair of damaged cells
- Anti-inflammatory mechanisms – reduce the inflammatory immune response to the brain injury
- Neurotrophic – promote cell survival and foster proliferation of existing cells
Safety:
Stem Cell tourism is unregulated and potentially dangerous.
No Stem Cell treatment is approved for use for CP anywhere in the world.
What is the data?
- 15 years of research
- 77 Clinical Studies
- 2427 people with CP treated – mostly children
- Mostly Phase 1 and Phase 2 studies, No Phase 3 of Any type
- Most well researched is on umbilical cord blood
The results are showing short term safety and compared to standard care, shows a slight but statistically significant improvement on gross motor function. However, current motor interventions such as botulinum toxin or CIMT have comparable effects
Takeaway - While promising, most studies are small-scale and lack long-term efficacy data. No Phase 3 trials have been published.
Considerations:
Discuss with healthcare providers, consider the lack of robust evidence, high costs ($10,000-updwards of $30,000), and be cautious of commercial claims, especially from unregulated overseas providers or from providers who are not medical doctors (such as chiropractors).
References:
Paton, M.C., Finch-Edmondson, M., Fahey, M.C., London, J., Badawi, N. and Novak, I. (2021), Fifteen years of human research using stem cells for cerebral palsy: A review of the research landscape. J Paediatr Child Health, 57: 295-296. https://doi.org/10.1111/jpc.15329
Eggenberger S, Boucard C, Schoeberlein A, Guzman R, Limacher A, Surbek D, Mueller M. Stem cell treatment and cerebral palsy: Systemic review and meta-analysis. World J Stem Cells 2019; 11(10): 891-903 [PMID: 31692977 DOI: 10.4252/wjsc.v11.i10.891]
What is the intervention:
Neurcytonix promotes a device known as the Neurocytotron, claiming it can “rewire” the brain and significantly improve neurological conditions such as cerebral palsy and hypoxic-ischemic encephalopathy.
How does it work?
According to its marketing, the device stimulates neurogenesis and cellular repair using low-frequency radio energy. However, there is no peer-reviewed scientific evidence to support these claims. The treatment is not approved by any major regulatory body, and its benefits remain unproven.
Who is it for?
Those with neurological conditions such as cerebral palsy and hypoxic-ischemic encephalopathy.
Is it safe?
What is the data?
A single, Randomized, double-blinded, placebo-controlled clinical trial evaluating the Neurocytotron was registered on ClinicalTrials.gov under the identifier NCT03743623. The trial began in March 2019 and ended in December 2022 with an enrollment of 53 pediatric participants diagnosed with cerebral palsy
Despite the trial’s completion, no data has been posted. There are no published results, no summary of findings, and no statistical analysis available to the public. Searches across PubMed, Google Scholar, and other academic databases confirm that there are no peer-reviewed articles authored by Neurcytonix researchers documenting methodology or clinical outcomes.
This absence of evidence means there is no way to evaluate the safety, effectiveness, or credibility of the treatment. Without publicly available results or peer-reviewed publications, the scientific community has no means to validate the claims being made.
Considerations:
- Cost of Treatment: The financial burden placed on families is significant. Based on available information, the Neurocytonix procedure costs 55,000 US dollars for the initial treatment. If additional sessions are requested or recommended, each follow-up treatment costs 35,000 US dollars. These charges are being applied despite the absence of any published clinical data verifying effectiveness or long-term outcomes.
- Travel: The treatment is offered in Mexico and requires at least a 28 day stay.
Families are asked to pay these costs without access to scientific proof, standardized treatment protocols, or evidence of benefit. This raises serious concerns about transparency, informed consent, and potential exploitation.
- The device is not approved or cleared by the Food and Drug Administration or any comparable international authority
- Media and Advocacy Commentary: Public awareness of Neurcytonix increased following its mention in the Netflix documentary Lucca’s World. The film features a child with HIE reportedly undergoing Neurocytotron treatment. However, no clinical data or evidence is provided to support the story.
References:
- ClinicalTrials.gov. Functional Neurogenesis Stimulation for Children With Cerebral Palsy. Study Identifier NCT03743623. Available at https://clinicaltrials.gov/study/NCT03743623
- Science-Based Medicine. Cytotron and Related Devices. Available at https://sciencebasedmedicine.org/cytotron-magical-device-pseudoscience
- The Guardian. With a New Hit Film, Netflix Has Reduced Disabled Lives to Feelgood Fodder. Available at https://www.theguardian.com/commentisfree/2025/feb/11/netflix-film-disabled-lives-feelgood-child-cerebral-palsy-families
- Hope for HIE. Lucca’s World on Netflix Brings Representation to HIE and Cerebral Palsy. Available at https://hopeforhie.org/luccas-world-on-netflix-brings-representation-to-hie-cerebral-palsy
- SmartPatients. Neurocytotron CP Trial Summary. Available at https://www.smartpatients.com/trials/NCT03743623
What is the intervention?
Use of “therapist-guided” or facilitated movements to provide sensory input and improve postural control.
Who is it for?
Babies and young children with neurodevelopmental disabilities such as Cerebral Palsy.
How does it work?
Child is relatively passive. The therapists facilitate normal movement and inhibit abnormal movement
Is it Safe?
Yes
What is the data?
NDT is well researched and consistent, strong evidence shows that NDT does not improve contracture and tone, weak evidence that NDT improves function.
Compared to other modalities, it has been found that Casting superior treatment for contracture management and Botulinum Toxins (BoNT) are more effective than NDT for tone reduction
Considerations:
NDT is expensive and time consuming.
References:
Final Thoughts:
Evaluating treatments and therapies for cerebral palsy requires a thoughtful and critical approach. By considering the source, claims, safety, efficacy, and practicality of a therapy, and by asking the right questions to healthcare providers and therapists, families can make informed decisions that best support their child's health and well-being. Always prioritize therapies backed by robust evidence and consult with healthcare professionals to ensure that any new approach complements existing care.
Additional References:
- Sowdhamini S. Wallace, Gal Barak, Grace Truong, Michelle W. Parker; Hierarchy of Evidence Within the Medical Literature. Hosp Pediatr August 2022; 12 (8): 745–750. https://doi.org/10.1542/hpeds.2022-006690
- Flaherty RJ; A simple method for evaluating clinical literature. Fam Pract Manag. 2004;11(5):47-52
- Novak, I., Mcintyre, S., Morgan, C., Campbell, L., Dark, L., Morton, N., Stumbles, E., Wilson, S.-A. and Goldsmith, S. (2013), A systematic review of interventions for children with cerebral palsy: state of the evidence. Dev Med Child Neurol, 55: 885-910.
- Novak, I., Morgan, C., Fahey, M. et al. State of the Evidence Traffic Lights 2019: Systematic Review of Interventions for Preventing and Treating Children with Cerebral Palsy. Curr Neurol Neurosci Rep 20, 3 (2020).
- Livingstone A, Servais L, Wilkinson DJC. The ethics of crowdfunding in paediatric neurology. Dev Med Child Neurol. 2023; 65(4): 450–455. https://doi.org/10.1111/dmcn.15442